For the millions living with diabetes, managing the condition is a daily reality. It involves monitoring blood sugar, making careful dietary choices, staying active, and sometimes, taking medication. While most people are aware of how diabetes affects the heart, kidneys, and eyes, one of the most significantly impacted—and often overlooked—areas is the feet. The connection isn’t random; it’s a direct consequence of how high blood sugar levels wage a silent war on your body’s intricate systems. Understanding this link is the first and most crucial step in preventing serious, life-altering complications.
This article will look at the direct impact of blood sugar on foot health, explain the mechanisms of damage, and provide a proactive playbook for daily care. Your feet carry you through life; it’s time to give them the attention they deserve.

How High Blood Sugar Harms Your Feet
High blood sugar doesn’t just cause one problem for your feet; it launches a two-pronged attack that compromises their structure and function. The two main culprits are diabetic neuropathy and peripheral artery disease.
Diabetic Neuropathy: The Nerve Damage Dilemma
Prolonged exposure to high blood sugar is toxic to your nerves. The most common form of nerve damage in diabetes is peripheral neuropathy, which affects the nerves in your extremities, especially the feet and legs. An estimated 40.3% of patients with diabetes are affected by this condition.
Imagine the nerves in your feet are like sophisticated electrical wiring that sends signals—like pain, heat, and cold—to your brain. Hyperglycemia corrodes this wiring, causing the signals to become weak, distorted, or to fail completely. This can lead to a range of symptoms:
- Tingling or a “pins and needles” sensation.
- Sharp, shooting pains or cramps.
- Extreme sensitivity to touch.
- Muscle weakness in the feet.
- Numbness or a complete loss of feeling.
The loss of sensation is the most dangerous aspect. Without the warning signal of pain, you might not notice a small cut, a blister from a poorly fitting shoe, or a pebble you’ve stepped on. You could burn your foot in hot water without realizing it. This lack of feedback turns minor, easily treatable issues into potentially severe threats.
Peripheral Artery Disease (PAD): The Circulation Crisis
Just as it damages nerves, high blood sugar also harms your blood vessels. It contributes to atherosclerosis, a condition where plaque (a sticky substance made of fat, cholesterol, and other materials) builds up inside the arteries. This narrows the vessels and hardens them, restricting blood flow. When this occurs in the arteries leading to your limbs, it’s called Peripheral Artery Disease (PAD).
Think of your circulatory system as the plumbing in a house. PAD is like a severe clog in the pipes leading to the furthest rooms—your feet. This “clog” means your feet don’t receive enough oxygen-rich blood. The consequences are significant:
- Slowed Healing: Wounds, cuts, and sores take much longer to heal because the necessary blood cells, oxygen, and nutrients can’t reach the site efficiently.
- Increased Infection Risk: A compromised blood supply weakens the immune response in the area, making it harder for your body to fight off bacteria.
- Painful Cramping: You might experience pain in your calves when walking (a condition called claudication) that subsides with rest.
- Physical Changes: The skin on your feet might become shiny, you could lose hair on your toes and feet, and your toenails might thicken or grow more slowly.
When you combine the nerve damage from neuropathy with the poor circulation from PAD, you create a perfect storm for serious foot complications.
How Foot Complications Escalate
The journey from a small blister to a major medical emergency can happen shockingly fast for someone with diabetes. Here’s how it typically unfolds:
1. The Unnoticed Injury: A person with neuropathy gets a small cut, blister, or ingrown toenail but feels no pain and is unaware of the injury.
2. The Healing Process Fails: Due to PAD, the wound receives inadequate blood flow. Instead of healing quickly, it remains open.
3. Infection Sets In: The open sore becomes a gateway for bacteria. The impaired circulation also means the body’s infection-fighting white blood cells can’t get to the wound effectively.
4. An Ulcer Develops: The persistent, infected, and non-healing wound can break down the skin and underlying tissue, forming a diabetic foot ulcer.
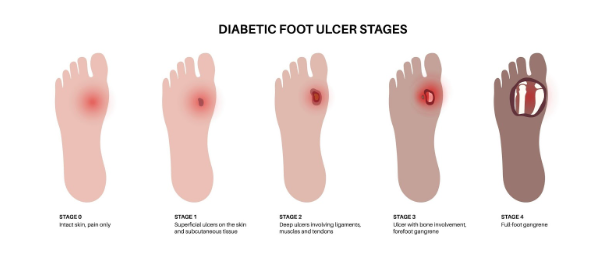
Licensed by Google
5. The Risk of Amputation: If the infection spreads to the surrounding tissue and bone (a condition called osteomyelitis) and cannot be controlled with antibiotics or other treatments, it can lead to tissue death (gangrene). At this stage, amputation of a toe, the foot, or even part of the leg may be necessary to save the person’s life.
This frightening cascade of events is why proactive, daily foot care is not just a good idea—it’s a non-negotiable part of diabetes management.

A Daily Routine for Healthy Feet
The best defense is a great offense. Integrating a simple foot care routine into your day can drastically reduce your risk of complications.
- Inspect Your Feet Daily: Set aside a specific time each day, like when you take off your shoes in the evening, to thoroughly check your feet. Look at the tops, soles, heels, and between your toes. Use a mirror or ask a family member for help if you can’t see the bottoms of your feet. Check for cuts, sores, blisters, redness, calluses, or any changes.
- Wash and Dry Carefully: Wash your feet daily with lukewarm—not hot—water. Test the water temperature with your elbow first. Use a mild soap. Afterward, dry your feet by gently patting them. Make sure to completely dry the areas between the toes to keep fungal infections at bay.
- Moisturize, But Not Between the Toes: Apply a thin layer of lotion to the tops and bottoms of your feet. This helps keep the skin on your feet soft, preventing cracks. Avoid putting lotion between your toes, as the extra moisture can encourage fungal growth.
- Care for Nails Properly: Cut your toenails straight across and gently file any sharp edges with an emery board. Avoid cutting the nails too short or rounding the corners, as this can lead to ingrown toenails. If you have trouble with your nails, see a podiatrist.
- Always Wear Shoes and Socks: Never go barefoot, even indoors. A stray object on the floor could cause an injury you won’t feel. Wear well-fitting, comfortable shoes and clean, dry socks. Change your socks immediately if they get wet or damp.
- Keep the Blood Flowing: When you’re sitting down, put your feet up. Wiggle your toes and move your ankles up and down for a few minutes. Do this several times a day. Avoid crossing your legs for long periods.
The Role of Your Healthcare Team and Lifestyle
Foot care doesn’t happen in a vacuum. It’s one piece of the comprehensive puzzle of diabetes management.
The single most effective way to protect your feet is to manage your blood sugar levels. By keeping your glucose within your target range through diet, exercise, and medication, you can slow down or even prevent nerve and blood vessel damage.
Furthermore, overall health plays a critical role. Factors like poor sleep can negatively impact blood sugar control and immune function. If you struggle with rest, a professional sleep assessment can identify underlying issues and help improve your metabolic health, which in turn benefits your entire body, including your feet.
Finally, establish a relationship with your healthcare team. This includes scheduling a comprehensive foot exam with your doctor or a podiatrist at least once a year. They can spot problems you might miss and provide specialized care.
When to Seek Immediate Help: Red Flags for Your Feet
Contact your doctor immediately if you notice any of the following:
- A cut, blister, or bruise on your foot that isn’t healing.
- Skin on your foot that is red, warm, or swollen.
- A callus with dried blood inside it.
- An infection or a sore that has become black and smelly.
- Pain, tingling, or numbness in your feet.
Taking the right steps today can ensure a healthier, more active future. At HOW Clinics, a premier wellness clinic in Guelph, we believe in a holistic and proactive approach to health. We are dedicated to empowering you with the knowledge and tools to manage your diabetes effectively and protect your long-term well-being.
Don’t wait for a small problem to become a serious one. If you have questions about diabetes management or foot care, take the first step. Call HOW Clinics today at 519-340-2744 to schedule a consultation.

